Diabetes Management Needs to Become Digital
Diabetes is quickly becoming an epidemic. If we don't act preventively the burden on healthcare will be too big. One of the solutions is to use digital technology in managing it.

This year marks the 100th anniversary since the discovery of insulin, which “transformed type 1 diabetes (DT1) from a fatal diagnosis into a medically manageable chronic condition”. But there’s still much we can do to improve the lives of 32 million people that live with diabetes in the EU. There are reports that 1 in 11 adults is living with type 2 diabetes (DT2). The challenge today is achieving optimal levels of glucose, preventing DT2 and preventing or delaying its complications.
Living with a chronic condition is certainly a burden, but many complications of DT1 and DT2 still arise from patient carelessness, lack of knowledge or motivation. The doctor’s presence is certainly of great help, but with the rapidly rising number of cases with this chronic condition (especially DT2), there are simply not enough of them. The only logical steps are better education about the disease, its management and consequences, and technology. And at Medical Notes we’ll focus on the latter.
As contextually mentioned earlier, diabetes is largely dependent on patient self-management and empowerment. Patients have to make countless decisions every day as to when to exercise, what to eat and timing the correct dosage of insulin. Additionally, if the data is collected, it can be done so from multiple sources - blood glucose measurements (such as CGMs), fitness trackers, insulin pumps, genomic, proteomic and metabolomic data and many more. The key is to integrate, analyse and present the data to the patient with personalised recommendations on how to act.
In essence, there are three major areas where digital health could enter diabetes care: diagnosis, treatment and long-term care.
Diagnosis
I already wrote about this in issue 31, but the newsletter was still in its early stages and poorly defined. Here’s a refreshed perspective on that.

Traditional diagnosis of DT2 is pretty straightforward. Based on one’s blood glucose levels, the patient either has diabetes or requires an oral glucose tolerance test (OGTT) to either confirm diabetes or pre-diabetes. Combine this method with measurements of glycated hemoglobin (HbgA1c) and you get a very reliable way of detecting hyperglycemia and ultimately diagnosing diabetes. Distinguishing between DT1 and DT2 is just a check for autoantibodies away.
The biggest problem is that diabetes (especially DT2) is becoming an epidemic. As mentioned in the beginning, 32 million people in the EU are living with it, along with about 10% of Americans. Some papers suggest this number to rise to 54 million in the USA by 2030. This is just too big of a burden for healthcare to keep up. By far the most effective way is to be preventive, but reducing the amount of sugar we consume in such a short time seems like too big of a challenge.
So, if we have to live with it, we have to find the most effective way of managing it. The continuous emergence of new at-home blood testing kits (GenePlanet, Everlywell, etc.) is a step in the right direction, as it offers an elegant way to measure blood biomarkers without ever having to leave one’s house.
But one of the promising and latest ideas for diagnosing diabetes is photoplethysmography (PPG), which “is a non-invasive optical technique that detects blood flow changes through a vascular bed”. A paper in August 2020 called this “a digital biomarker for diabetes” as it could be used as a smartphone app. The potential here is detecting diabetes earlier by screening for it, which is currently not recommended. I hope better detection is at least partly why the number of cases will increase so much in the following decade.
Treatment and long-term care
Assuming a patient is receiving insulin treatment, the biggest problem is that it’s hard to exactly know when and how much insulin to inject. And this is variable, especially because of meals and exercise. The complications because of this could be diminished to some extent with technology.
In September 2020, a paper was published in Nature Medicine that tested a decision support system (DSS) called ADVICE4U that could assist patients in administering insulin. They concluded that patients administering insulin by themselves using ADVICE4U do not result in worse glycemic levels than when they do this under doctor supervision. This could be a great solution in addition to the possibility of screening for diabetes.
Treatment and long-term care are, of course, interconnected, as diabetes is a chronic condition. If the number of diabetics will increase as the projections show hospital capacities will not follow and diabetics still have to have some sort of doctor’s visits. It seems the best solution for this is virtual hospital visits, which are perfect for managing chronic conditions.

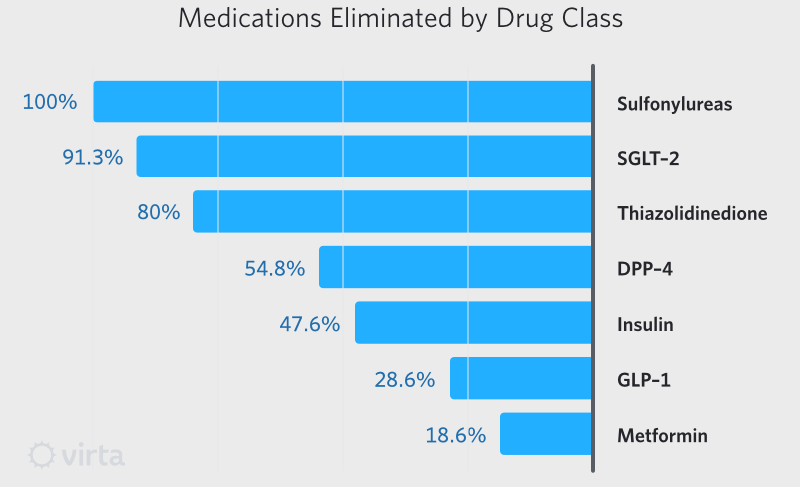
A startup caught my eye that’s called Virta Health and is trying to solve long-term diabetes care. However, they approach it differently, as their mission is to manage DT2 without using insulin or any other medication. In fact, their primary goal is to get patients off medication. They achieve this by helping people lower blood sugar and lose weight and even claim they can even help reverse DT2 (referring to reversing the prediabetic state).
Virta Health provides online medical care by physicians in addition to offering an app to patients. Most importantly, they personalise every aspect of patient care, from nutrition to behaviour. It’s more like a coaching service than doctor’s appointments. Read more about how it works.
At one year, clinical trial patients eliminated 63% of diabetes-specific medications. 94% of patients eliminated or reduce insulin usage. - Virta Health
They did extensive research into the benefits of their programme and the results look fantastic because it’s not only DT2 they’re managing, but also reducing the impact of its consequences. Here are the outcomes briefly:
- Lower HbA1c, glucose, insulin concentration, medication and improved insulin resistance
- Reduction of obesity among participants
- Improvement of TG/HDL ratio
- Reduced blood pressure and the need for medication
- Less inflammation
- No hypoglycemic events and improved cardiovascular risk markers
The tools and ideas are there, and new ones are always in development. We have the technology. Startups like Virta Health are on a mission to manage DT2 without medication. The only thing we have to do is apply it. Let’s not make this the biggest barrier.